KA Imaging’s Reveal 35C is a solution for better mobile imaging – especially in challenging environments like the ER. The Reveal 35C X-ray detector provides high-quality DR images (up to 75% DQE), with the added benefit of offering dual-energy images in mobile applications. It uses the same dose, same source and same workflow as a regular X-ray. Reveal’s dual-energy images can be used for better visualization of line and tube tips, retained surgical objects, pneumothorax, bedside pneumonia, among other applications. Read this interview with KA Imaging’s CTO Dr. Karim S Karim to learn more.
What is the difference between a mobile dual-energy X-ray system and a mobile or fixed regular X-ray system?
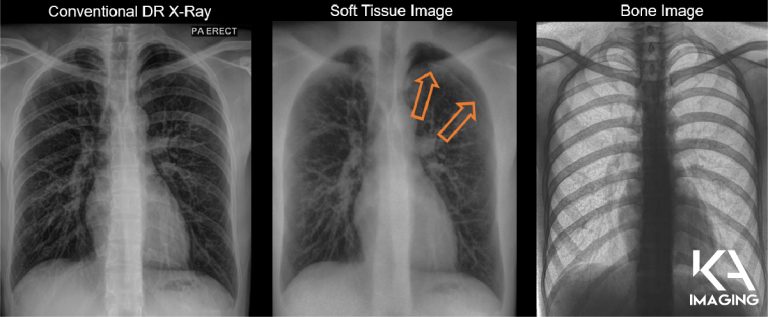
Karim S. Karim, CTO of KA Imaging: The biggest difference with dual energy is that you get better discrimination of soft tissue and bone. With the Reveal 35C technology we’re getting a regular X-ray, plus a soft tissue image and a bone image. The advantage of these spectral images, the soft tissue and the bone, is that you can visualize soft tissue without interference from the bone. You can visualize bone without interference from the soft tissue. For example: in the bone image you can see lines, tubes and calcified nodules beautifully; in the soft tissue image you can see pneumothorax and pneumonia quite nicely.
In the past, if you wanted to improve the material differentiation of mobile or fixed X-rays, you would have to buy a software that would let you visualize lines and tubes; and then you would have to get another software that would let you visualize nodules; and then you would have to get a third software that would let you visualize pneumothorax… In fact, if you look on the market, you have a lot of vendors selling all these specialized software as separate pieces whereas with our KA Imaging spectral dual energy X-ray imaging, you get all of those benefits already integrated. You don’t need to go out and get a special software for each use case.
An X-ray image that improves the overall visualization will reduce the chance that small abnormalities would be missed, which means better outcomes for the patient and hospital. Also, spectral imaging lets you identify materials that regular X-ray imaging would not be able to. So for example, something that shows up in the bone image most likely is calcified like a calcified nodule, a calcified artery, a calcified vessel, and something that shows up in the soft tissue is soft tissue. In regular X-ray, you have to guess if a nodule is calcified or not. By material discrimination, you add an additional layer of analysis and data for the clinician, and it allows the clinician to make a better decision than they would if they were just looking at regular X-ray imaging, mobile or fixed.
There are some dual energy solutions for fixed rooms. However, it’s the first time it can be used in mobile settings. What are the benefits of dual energy for mobile imaging?
KK – The biggest challenge for fixed dual-energy imaging is that the patient has to be ambulatory or able to go for the imaging. If you think about fixed X-ray imaging, people might even argue that you “can just get a CT.” However, a CT is 50 times the radiation dose of a regular X-ray. Sometimes – when a patient is in the ICU for example – you don’t have the alternative to get a CT because the patient cannot go to the X-ray room, so the X-ray must come to the patient. It’s not possible to move an ICU patient for a CT all the time! This means that good quality mobile X-ray is essential. Not only good quality regular DR, but good soft tissue differentiation as well.
In addition, in rural and remote parts of North America, you don’t have access to CT. It is just not available. And so the advantage of having dual energy or spectral imaging in the mobile for the first time is that you’re going to get better clinical outcomes. With better differentiation than a regular X-ray, and without extra radiation dose, without the fixed infrastructure and without the high cost.
What types of patients would benefit from the technology?
KK – In a sense, I would say that mobile dual-energy X-ray today has some very prominent use cases. The first use case is for those patients that are bedridden. In this category you would have patients in the intensive care unit, patients in for example the neonatal or pediatric ICU, patients in the cardiac critical care units, right, people who cannot basically go for an X-ray or go for a CT.
 You also have patients in long term care facilities, some experiencing mobility issues, they can’t really go around to be imaged. Imaging must go to them.
You also have patients in long term care facilities, some experiencing mobility issues, they can’t really go around to be imaged. Imaging must go to them.
Another interesting use case is prisons. If you’re trying to do any kind of screening of disease there, you can’t very well take a CT to that patient. So again, a portable solution is where the value comes in.
Screening or triaging for general population is also an interesting application. If you’re trying to triage cardiac disease or lung cancer or tuberculosis or even pulmonary fibrosis… Any other kind of occupational health disease. In those situations, using CT is not the right solution because the radiation dose is very high and if you’re screening such a large general population, the radiation dose to that population will be unacceptable. Even with LDCT, you are still looking at 10X to 20X more radiation than a standard AP X-ray so the ALARA principle would guide us to use the lowest dose modality that can provide a good outcome. There is also a limitation in terms of access to LDCT as well as infrequent follow ups because patients are concerned about CT dose, as we know… In those situations, a mobile Reveal system again can be quite valuable. Because it’s mobile, because it’s portable, it can be used in screening centers that are distributed across, without having to be concentrated just in hospitals. There could be units in long term care facilities, they could be in mobile vans, they could be in rural and remote areas… And that’s where the screening element becomes quite valuable.
What is the impact for rural and remote communities?
KK – The biggest challenge for these communities is access. The second piece that’s challenging for these communities is not just access to equipment, but also access to qualified radiologists, qualified clinicians to make a timely diagnosis. So even though one could argue that we can send the images to be read overseas or to be read using teleradiology, the question is in some situations you need a diagnosis instantly. For example, if I’m in a rural community in the ICU and I’ve got a pneumothorax, I need that diagnosis immediately because waiting for three hours may cause a very serious change in the patient condition.
These are also situations where spectral imaging combined with, for example, some kind of artificial intelligence or computer aided diagnosis could enable an instant diagnosis. It’s something that regular X-ray couldn’t do because it doesn’t have that material classification and identification capability that spectral imaging does. So it’s not just about access to equipment, it’s also access to a timely diagnosis.